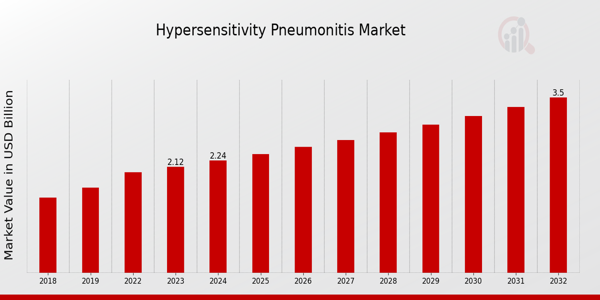
As we navigate the evolving landscape of respiratory medicine in 2025, I've witnessed remarkable advancements in how we approach Hypersensitivity Pneumonitis (HP). You might be wondering how these developments affect your practice and patients. Today, I'm sharing the latest insights on early detection, management strategies, emerging research, technological innovations, and fundamental understanding of HP that every healthcare professional should know.
Understanding Hypersensitivity Pneumonitis: A 2025 Perspective
Hypersensitivity Pneumonitis continues to challenge healthcare providers with its complex presentation. You've likely noticed the rising incidence rates in certain geographic regions. This inflammatory lung condition, triggered by repeated inhalation of specific antigens, presents differently among patients. The classification system has evolved, with acute, subacute, and chronic forms now supplemented by additional subcategories based on molecular signatures.
Diagnosis relies on a combination of clinical presentation, exposure history, radiographic findings, and sometimes lung biopsy. I've found that early identification dramatically improves outcomes. The immunological mechanisms underlying HP have become clearer through advanced research. These insights have revolutionized our approach to treatment.
Early Detection Strategies Transforming Patient Outcomes
Early detection of Hypersensitivity Pneumonitis has transformed dramatically. You now have access to more sensitive biomarkers that indicate lung inflammation before symptoms appear. These biomarkers help identify disease activity and guide treatment decisions. Non-invasive breath analysis technologies have advanced significantly, offering immediate results in clinical settings.
High-resolution CT protocols specifically designed for HP detection have improved visualization of subtle lung changes. These protocols use lower radiation doses while maintaining excellent image quality. Mobile screening units bring advanced diagnostic capabilities to remote areas. Artificial intelligence algorithms now assist in pattern recognition on imaging studies with impressive accuracy.
The current approach to early detection includes:
- Multi-biomarker panels analyzing inflammatory mediators in blood samples
- Specialized pulmonary function testing protocols detecting subtle functional changes
- Home monitoring devices enabling continuous respiratory assessment between clinic visits
- Genetic screening panels identifying predisposition to specific antigen sensitivities
- Portable point-of-care diagnostic tools delivering results within minutes
Groundbreaking Research Reshaping Prevention Strategies
Research breakthroughs have revolutionized our understanding of Hypersensitivity Pneumonitis. The genetic factors predisposing individuals to HP have been mapped extensively. You can now access personalized risk assessment tools incorporating genetic data, occupation, and environmental factors. Immunomodulation strategies target specific pathways without comprehensive immunosuppression.
Preventive environmental interventions have proven highly effective when implemented early. Workplace monitoring technologies have advanced significantly, detecting potential antigens before exposure reaches harmful levels. Remote sensing technologies identify environmental triggers with remarkable precision. These developments have shifted our approach from reactive treatment to proactive prevention.
Technological Innovations Making Breathing Easier
Technology has transformed HP management in ways previously unimaginable. Smart home systems continuously monitor air quality and alert residents to potential triggers. Wearable devices track respiratory parameters and provide early warning of exacerbations. You've likely integrated some of these innovations into your clinical practice already.
Telemedicine platforms specifically designed for respiratory disease management facilitate regular check-ins without hospital visits. Virtual reality programs train patients in proper use of respiratory equipment and medication delivery. Machine learning algorithms predict exacerbations based on environmental data and patient activity patterns.
Comprehensive Management Approach: From Diagnosis to Long-term Care
The management landscape for Hypersensitivity Pneumonitis has evolved dramatically. Treatment now follows personalized protocols based on phenotyping and endotyping. Targeted biological therapies address specific inflammatory pathways with fewer side effects. Pulmonary rehabilitation programs incorporate cutting-edge techniques for optimal recovery.
| Management Aspect | Traditional Approach (Pre-2023) | Current Approach (2025) |
|---|---|---|
| Diagnosis | Primarily symptom-based with supportive imaging | Multi-modal approach with molecular phenotyping |
| Antigen Identification | Limited panel testing | Comprehensive environmental assessment with molecular analysis |
| Treatment Selection | Standardized protocols based on disease severity | Personalized approach based on molecular endotypes |
| Monitoring | Periodic clinic visits with pulmonary function tests | Continuous remote monitoring with AI-assisted trend analysis |
| Rehabilitation | General exercise programs | Personalized protocols with virtual coaching |
| Environmental Management | Basic avoidance strategies | Smart environmental control systems with predictive alerts |
The integrated approach to management has yielded substantially improved outcomes. Patients report better quality of life and reduced hospitalization rates. You'll find that early intervention based on molecular profiling prevents progression to chronic forms. Environmental modification strategies have become more sophisticated and effective.
Navigating Regulatory Changes Affecting HP Management
Regulatory frameworks have evolved to address emerging challenges in Hypersensitivity Pneumonitis management. Workplace safety guidelines now include more specific provisions for potential HP triggers. Insurance coverage has expanded for specialized diagnostic testing and innovative treatments. These changes directly impact how you provide care to your patients.
Standardized reporting systems track HP incidence across different industries and regions. The resulting data drives policy decisions and resource allocation. International collaboration has harmonized approaches to HP management across borders. These developments create new opportunities for implementing best practices in your setting.
Future Directions: Where We're Heading with HP Care
Looking ahead, several promising developments are on the horizon. Gene therapy approaches targeting susceptibility factors show early promise in clinical trials. You'll soon see advanced air filtration technologies becoming more accessible and affordable. The integration of artificial intelligence throughout the care continuum will continue to accelerate.
I believe we're moving toward a future where Hypersensitivity Pneumonitis becomes largely preventable through early intervention. Personalized approaches will continue to replace one-size-fits-all treatment strategies. The collaboration between environmental scientists, immunologists, and clinicians will yield innovative solutions to persistent challenges.
Conclusion: Embracing a New Era in Hypersensitivity Pneumonitis Care
The landscape of Hypersensitivity Pneumonitis diagnosis, management, and prevention has transformed dramatically. You now have powerful tools to identify at-risk patients, detect disease earlier, and implement more effective interventions. These advances offer hope to patients facing this challenging condition.
I encourage you to explore these innovations and consider how they might enhance your practice. The integration of advanced diagnostics, personalized therapies, and environmental management creates unprecedented opportunities for improving outcomes. Together, we can make Hypersensitivity Pneumonitis a more manageable condition with better long-term prognosis.